Article
Young Men Need More Medicaid

Article
Fact-based, data-driven research and analysis to advance democratic debate on vital issues shaping people’s lives.
Center for Economic and Policy Research
1611 Connecticut Ave. NW
Suite 400
Washington, DC 20009
Tel: 202-293-5380
Fax: 202-588-1356
https://cepr.net
Recent research establishes a link between losing Medicaid at age 19 and incarceration among young men. Using a research design that linked Medicaid records and criminal justice records for young low-income men in South Carolina, economist Elisa Jácome found that among the young men in her sample who were incarcerated before age 21, about 80 percent had a prior mental health diagnosis during adolescence, and that young men who lost Medicaid eligibility at age 19 were more likely to be incarcerated over the next two years than those in a matched comparison group. Her work builds on earlier research finding that access to mental health and substance abuse services reduces arrests and local crime rates, as well as a growing body of research on the importance of health insurance for young adults.
In this brief, we provide additional context for Jácome’s findings by documenting how common it is for young men to lose Medicaid eligibility and become uninsured during the transition to adulthood. We also discuss how to increase young men’s coverage during this crucial period. Most immediately, Congress can help young men, while narrowing class, racial, and ethnic disparities in coverage, by establishing a federal Medicaid program for adults living in states that have yet to expand to Medicaid. The House’s Build Back Better Act, legislation that is currently moving through Congress under budget reconciliation rules, would create such a program. Looking beyond this year, older boys and young men would benefit most from the kind of universal coverage that is common in most other wealthy nations.
About 95 percent of US children have health insurance coverage. Among insured children in 2020, about 37 percent had coverage through Medicaid. Most of the rest are covered as dependents through a parent’s employer-based coverage.
In nearly all states, children living in families with income below 200 percent of poverty (or even higher income levels in many states) are eligible for Medicaid until their 19th birthday. In South Carolina, for example, children are eligible for Medicaid (via the closely related Children’s Health Insurance Program) through age 18 as long as they live in a family with income below 208 percent of the federal poverty line, or just under $47,000 for a family of three.
Once a child turns 19, their Medicaid eligibility varies by their income and whether they live in one of the 39 states and the District of Columbia that have expanded Medicaid as allowed under the Affordable Care Act, or one of the 12 states that have not. In expansion states, non-elderly adults, including 19 to 25-year-olds, are generally eligible for Medicaid, but only if they have incomes below 138 percent of poverty, or $12,880 for an individual in 2021.
By contrast, the Affordable Care Act (ACA) requires private health plans and issuers that offer dependent child coverage to make such coverage available until a child reaches the age of 26. Thus, children covered as dependents under a parent’s employer-based or individual market coverage can typically stay on that coverage until their 26th birthday regardless of their income.
After the ACA’s dependent provision went into effect in 2010, the uninsurance rate among adults ages 19–25 fell from 36 percent to 27 percent. Research suggests that the provision resulted in increases in mental health treatment, reductions in out-of-pocket spending on health care, reductions in disease-related mortality, and various other health and financial improvements.
There is also evidence that “males experienced larger improvements in health-related outcomes from the ACA dependent coverage provision than females,” in part because gains in coverage and responses to obtaining coverage were larger among young men than young women.
At the same time, the ACA’s dependent coverage provision did not help close gaps in coverage by race and ethnicity. In fact, O’Hara and Brault found that “[n]et gains in coverage for non-Hispanic whites exceeded net gains in coverage for non-Hispanic blacks.” Similarly, Barbaresco and others found that “college graduates experienced greater improvements in health-related outcomes [after implementation of the dependent coverage care provision] than non-college graduates ….” By contrast, the ACA’s Medicaid expansion provision has contributed to increases in coverage among low-income young adults in expansion states, particularly low-income young adults who are Black, Hispanic, or do not have a college degree. Yet, as we document below, uninsurance rates continue to increase starting at age 18 because the loss of Medicaid coverage is not fully offset by increases in other coverage.
Table 1 uses data from the 2019 American Community Survey (ACS) to estimate health insurance status (covered by Medicaid, covered by private or other public health insurance, and not covered) by age for young men ages 16–24. As the table shows, about 32 percent of 16 and 17-year-old men are covered by Medicaid. The Medicaid coverage rate starts declining at age 18 and through age 22. Only between 12–13 percent of men in their early 20s have Medicaid coverage. While men in their early 20s are more likely to have other forms of coverage, these gains offset only about half the decline in Medicaid coverage, so young men’s uninsurance rate more than doubles by age 20.
| Age | No Health Insurance Coverage | Medicaid | Other Health Insurance |
|---|---|---|---|
| 16 | 7% | 32% | 61% |
| 17 | 8% | 32% | 60% |
| 18 | 10% | 26% | 63% |
| 19 | 15% | 18% | 68% |
| 20 | 17% | 15% | 68% |
| 21 | 18% | 13% | 69% |
| 22 | 18% | 12% | 70% |
| 23 | 17% | 13% | 70% |
| 24 | 17% | 12% | 71% |
| 25 | 18% | 12% | 71% |
Source: Authors’ analysis of American Communities Survey using IPUMS-USA.
Figures 1 and 2 break out these health insurance coverage estimates by race and ethnicity. For these estimates, we use five years of data from the ACS to obtain reliable estimates by age for each group.
As Figure 1 shows, only about 4 percent of white boys are uninsured at age 16. Both Black and Asian/Pacific Islander boys have slightly higher uninsurance rates (about 6 percent), while both Hispanic and American Indian/Alaskan Native boys have much higher uninsurance rates, roughly 12 and 18 percent, respectively, at age 16.
Figure 1 also shows how uninsurance increases during the transition to adulthood for men in all of these racial and ethnic groups. At age 22, about 25 percent of Black men, 30 percent of Hispanic men, and 33 percent of American Indian/Alaskan Native men are uninsured.
Figure 1
Figure 2
As Figure 2 shows, Medicaid plays a crucial role in reducing uninsurance among 16 to 18-year-old boys in all groups, but it is especially important for Black, Hispanic, and American Indian/Alaskan Native boys. About half of Black 16-year-olds are covered by Medicaid, as are just under half of Hispanics, compared to about one-in-five whites. However, Medicaid coverage drops sharply at age 18 for all groups.
Uninsurance rates for young men are particularly high in states that have not expanded Medicaid. In the 31 states, including the District of Columbia, that had adopted Medicaid expansion by January 1, 2016, we found that about 13 percent of 19 to 25-year-olds were uninsured compared to just over 23 percent of 19 to 25-year-olds in the states that had not adopted Medicaid expansion by then. Recent research suggests that the American Community Survey may undercount Medicaid enrollment in states that have expanded Medicaid, so the actual uninsured rate in the 31 states that had adopted Medicaid expansion by 2016 may be lower than 13 percent.
Figure 3 shows uninsurance rates in the 10 most populous US states. The first four states in the figure have not expanded Medicaid; the remaining six states have expanded it. As with the overall state data, young men’s likelihood of being uninsured more than doubles in all states during the transition to adulthood, but uninsurance is particularly high for young men in the four non-expansion states.
Figure 3
Although the focus of this piece is on boys and men, loss of Medicaid and other forms of coverage is also a major problem for girls and women. As CEPR has previously documented (see Figure 4, below), white boys, Black boys, Black girls, and white girls all have roughly the same relatively low rate of uninsurance during childhood. However, their uninsurance rates spike and diverge considerably starting in young adulthood.
Figure 4
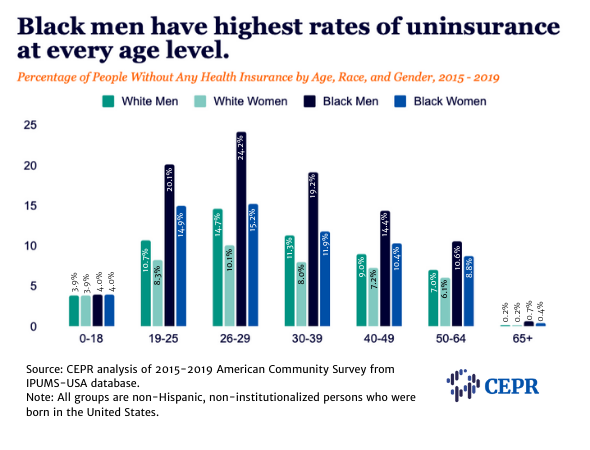
The absence of universal health coverage, and other broadly inclusive social protections, has done considerable harm to boys and men in the United States. As CEPR has previously argued, the lack of such protections is likely due in part to policymaking based on stereotypical assumptions about men, particularly Black men.
Much more needs to be done to ensure that all adolescents, regardless of gender, have stable, continuous health insurance during and after the transition to adulthood. Most immediately, Congress should pass legislation that would create a federal Medicaid program for adults living in states that have yet to expand Medicaid. This legislation is currently included in the Build Back Better Act moving through Congress under the budget reconciliation process.
Looking forward, young people would benefit most from the kind of universal coverage that is common in most other wealthy nations. In addition to ensuring coverage for all, this would reduce the considerable administrative burdens that make it difficult for many otherwise eligible people to obtain and maintain coverage that is means-tested or based on falling into a particular category.
The authors thank Algernon Austin for helpful comments on a draft of this article.