October 25, 2024
By feigning a desire to improve seniors’ health while actually prioritizing squeezing as much profit as possible, private insurance giants like UnitedHealthcare and CVS – which receive taxpayer funds to provide Medicare Advantage (MA) plans – are engaging in a dangerous, thoroughly deceitful scam. The previous sentence is not conjecture – it comes from the companies’ own internal communications.
On October 17, the US Senate Permanent Subcommittee on Investigations published a report detailing how MA companies deny health coverage for American seniors, particularly post-acute care. The report focuses on the leading insurance giants – UnitedHealthcare, Humana, and CVS – which accounted for 59% of all MA enrollees in 2024. These companies denied prior authorization requests for post-acute care (like skilled nursing facility stays) at significantly higher rates than other types of care from 2019 to 2022. For example, UnitedHealthcare denied coverage requests for post-acute care at an 8.7% rate in 2019; by 2022, that denial was 22.7% – meaning the company denied more than one in five requests.
“Utilization Management” – Or, Denying Health Care
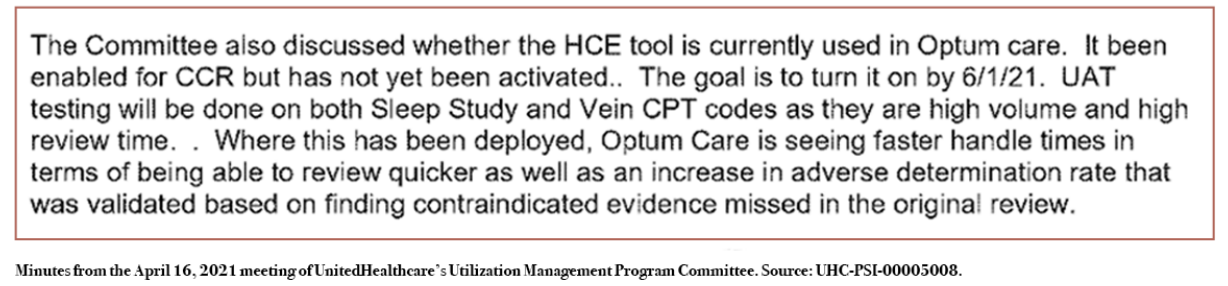
As part of this investigation, the subcommittee acquired internal company documents revealing the explicit intentions of corporate executives. Notes from an April 16, 2021 meeting among UnitedHealthcare’s internal committee on “utilization management” touted the benefits of Machine-Assisted Prior Authorization (MAP) technology. Along with quicker review times, the committee highlighted the “increase in adverse determination rate[s]” – in other words, an increase in denying American seniors the healthcare coverage that taxpayers are paying those companies to provide. The committee’s name – the “Utilization Management Program Committee” – showcases the corporate focus on managing what care Americans get covered.
In January 2019, a committee within CVS produced a chart showing that the more prior authorization requests the company imposed on patients, the more money the company saved. In April 2021, CVS employed an artificial intelligence program to cover less post-acute care, later projecting that the initiative would save $77 million over three years. Notes from a March 2022 meeting showed that losses in savings would be “too large to move forward” if the company reduced the amount of prior authorizations it required.
Humana shared this focus on using care denials to keep as much taxpayer money for itself as possible. In December 2019, a lead medical director revised templates for corporate strategy on prior authorization denials, writing in an email that the revisions were “important for denial purposes.” From 2020 through 2021, Humana held four conferences that trained its MA prior authorization clinical review teams on when to deny requests for long-term acute care hospital (LTACH) admissions. Such conferences included advice on how to speak with patients’ providers about care denials, such as highlighting how LTACHs are a “high cost intervention” and giving providers a “gut check” by asking if they had a goals-of-care conversation with their patients.
Advertising Versus Reality
Unsurprisingly, the corporate focus on managing utilization (i.e. spending less on covering care) stands in sharp contrast to the cheerful commercials they push on Americans. One September 2023 UnitedHealthcare advertisement highlights the company’s large provider network and shows happy people who are able to get coverage for a diverse array of needs – whether it be at the pharmacy or to “keep my smile looking good.” A September 2024 ad shows happy seniors having fun with their families with cheerful music, citing the “reliable healthcare coverage from UnitedHealthcare.” Several Aetna (owned by CVS) advertisements tout the seemingly comprehensive vision, dental, and hearing coverage under their MA plans. Humana has advertised how it puts seniors in charge of their healthcare.
Substantively, there are significant issues with these advertisements. Nearly all health care providers accept Medicare (also known as Traditional Medicare), while Americans enrolled in MA plans – whether from UnitedHealthcare or any other private insurer – are stuck with limited networks. The supplemental benefits touted by MA plans are often quite poor, with high coinsurance rates and low annual dollar limits. Rather than providing reliable care that puts patients in charge of their healthcare, these MA plans literally restrict patients to certain groups of in-network providers – and then subject them to prior authorizations, delays, and denials.
The advertisements highlight how deceitful and untrustworthy these for-profit health insurance giants are. These companies are funded by taxpayers to provide American seniors with healthcare coverage. Unlike Medicare, which directly reimburses providers for provided services, these private insurers generally get paid per person they enroll, and they make money from what they save by not spending money on the beneficiaries they claim to serve. Thus, they are financially incentivized to spend as little as possible, rather than provide the comprehensive coverage they advertise.
Medicare “Advantage” Mythmaking
The private insurance corporations like to sell the idea that these plans work because they are incentivized to keep their patients as healthy as possible – which then consequently lowers healthcare spending. However, there is no strong evidence that the MA model has caused American seniors’ to get healthier. If anything, MA companies’ usage of prior authorizations can harm patient care. A 2022 survey of physicians found that 94% reported that prior authorizations caused delays to necessary care, with 56% saying this occurred always or often.
At the same time, Medicare Advantage has never saved taxpayers money. Americans have had to pay more to finance seniors’ health coverage than they would have if all beneficiaries were in Medicare. In fact, insurers like UnitedHealthcare, CVS, and Humana have exploited the system to reap significant overpayments from taxpayers. The Medicare Payment Advisory Commission (MedPAC) estimated $83 billion in overpayments in 2024 as a result of methods like upcoding – the practice of pretending patients are sicker to get more money – and favorable selection – choosing healthier patients. For 2022, the Physicians for a National Health Program (PNHP) estimated between $88-$140 billion in overpayments from such practices.
While increasing costs for taxpayers, MA has enriched insurance companies. In 2021, MA insurers took in $1,730 of gross profit per enrollee, more than twice their $745 profit margin on the individual market. As my colleague Emma Curchin documented, MA companies are reducing plan offerings, cutting benefits and raising copays and the cost burden – in large part because their customers are actually using the healthcare they are paying for. That’s not the only issue for MA insurers; CMS did not increase payments to the companies as much as they wanted for 2025. Also, the Inflation Reduction Act instituted a $2,000 cap on out-of-pocket expenses for prescription drugs in Medicare Part D, shifting the cost burden from patients more towards the insurance companies.
Overall, Medicare Advantage companies advertise to American seniors a grandiose vision of comprehensive, expansive health coverage that puts greater power into the hands of patients. Yet, these insurers’ actually seek to control what care patients get access to, and their own communications reveal their focus on profiting by limiting access to and denying coverage for requested care. Given that MA plans make money by spending less on health coverage, they have never saved taxpayers money, and they have reaped billions in overpayments, they are actually de facto stealing billions from Americans.
Given the situation, there are alternatives that policymakers can pursue. Many Americans choose to enroll in MA plans not because they provide great health coverage, but because Traditional Medicare has significant gaps. While the government requires that all MA plans provide an out-of-pocket cap on medical expenses, there is no such requirement for Medicare, which does not cover 20% of outpatient care along with other potentially financially-restrictive cost-sharing arrangements for inpatient care. Additionally, the program does not cover vision, dental, and hearing care.
The government could reallocate the many billions of dollars in overpayments to Medicare Advantage insurers to institute a $5,000 or even lower out-of-pocket cap for Medicare along with providing vision, dental, and hearing coverage as well.1 Unlike MA, patients would enjoy genuine control over their healthcare, since nearly every provider accepts Traditional Medicare, there are no prior authorizations, and CMS’ objective is not to profit by restricting access to care. The status quo – shoveling billions to private companies that seek to deny care for their own profits – is expensive for everyone, frustrating for doctors and caregivers, and confusing to patients who need the healthcare they deserve.