In an otherwise insightful article on how the medical system profits from surprise medical bills, medical doctor and journalist Elisabeth Rosenthal fails to mention the detrimental role played by private equity firms.1 Most patients don’t know that hospitals and physician’s practices negotiate separate contracts with insurers, and that it’s possible for a hospital to be in-network for an insured patient, but for a doctor that cares for them to be out-of-network. Emergency room doctors, anesthesiologists, radiologists — doctors that patients do not get to choose — are most likely to be out-of-network. Hospitals contract with doctors’ practices or with large physician staffing firms for these doctors. In these situations, patients do not get to choose their doctor and cannot select a doctor that is in-network. The doctors will see a steady stream of patients and will not lose business because their patients have been hit with surprise medical bills that may be hundreds or even thousands of dollars more than what their health insurance companies pay for the same care. A Stanford University study found that by 2016, 42.8 percent of trips to the ER — more than 4-in-10 — led to patients getting surprise medical bills.2
A recent study found that out-of-network billing by these medical specialists raises physician payments for privately insured patients and raises health care spending by $40 billion annually.33
TeamHealth and Envision are the two largest physician staffing companies in the US, and both are owned by private equity firms. The design of the private equity business model in health care drives up the costs of patient care. Private equity funds rely on the classic leveraged buyout model (LBO) in which they use substantial debt to buyout specialty physician practices. High debt means PE owners put up very little equity, and returns are multiplied if the investment is successful. Private equity targets companies like emergency medical practices that have a steady and high cash flow so they can manage the cash in order to service the debt and make high returns. Demand for these services is inelastic (not sensitive to price) and is high — almost 50 percent of medical care is delivered by emergency rooms, according to a 2017 national study.4 PE firms believe they face little or no downside market risk in these buyouts.
Private equity-owned physician staffing firms grow by buying up many small specialty practices and “rolling them up” into umbrella organizations that serve health care systems across the United States. KKR-owned Envision Healthcare with 69,300 employees, and Blackstone-owned TeamHealth with 20,000 employees, dominate the market for outsourced doctors’ practices. A team of Yale University health economists examined what happened when private equity-owned companies EmCare (part of Envision Healthcare) and TeamHealth took over hospital emergency departments.5 They found that when EmCare took over the management of emergency departments, it nearly doubled its charges for caring for patients compared to the charges billed by previous physician groups. The researchers also found that TeamHealth took a somewhat different tack. It used the threat of sending high out-of-network surprise bills for ER doctors’ services to an insurance company’s covered patients in order to gain high fees from insurance companies as in-network doctors.6 This avoids the situation where a patient gets stuck with a large, surprise medical bill, but it raises premium costs for everyone. In both cases, healthcare costs increase when outsourced emergency rooms and other physician services are owned by private equity firms.
Outrage from families saddled with medical debt despite having health insurance spurred Congress to act. Early in the summer of 2019, Congress appeared poised to protect consumers from surprise medical bills and to hold insured patients financially harmless in situations where they were unable to choose their doctor. Senators Lamar Alexander and Patty Murray introduced the bipartisan Lower Health Care Costs Act, a strong bill to rein in surprise bills. At about the same time, the House Energy and Commerce Committee took up the bipartisan No Surprises Act, introduced by Frank Pallone Jr. and Greg Walden. The chance that legislation would pass in 2019 to protect insured patients from high out-of-network charges looked good.
Two solutions, both of which take surprise charges to patients out of the equation, have been put forward. Employers, patient advocates, and insurance companies favor paying out-of-network doctors a rate “benchmarked” to rates negotiated with in-network doctors to hold down health costs. Not surprisingly, this solution is opposed by large physician staffing companies and specialist physician practices that want to continue to charge prices higher than the in-network fees. These doctors’ practices, some backed by private equity firms, have been lobbying intensively for a second option that would allow doctors dissatisfied with a negotiated rate to seek a higher fee via an arbitration process that they believe will ensure higher physician pay and higher company revenues and profits.7
The campaign by Physicians for Fair Coverage, a private equity-backed group lobbying on behalf of large physician staffing firms, launched a $1.2 million national ad campaign in July to push for this second approach.8 The lobbying campaign bore fruit. In July, Pallone and Walden accepted an amendment to allow arbitration, but only in special cases, and it required the arbitrator to use negotiated rates instead of provider charges when deciding on disputes over payment.9 But the private equity-owned physician staffing companies were not satisfied. In late July, a mysterious group called Doctor Patient Unity launched a $28 million ad and lobbying campaign (now up to nearly $54 million) aimed at keeping any legislation to protect patients from surprise medical bills from passing. In mid-September, a representative for Doctor Patient Unity finally revealed what many observers already suspected — that PE-owned doctor staffing firms Envision Healthcare and TeamHealth were behind the campaign.10
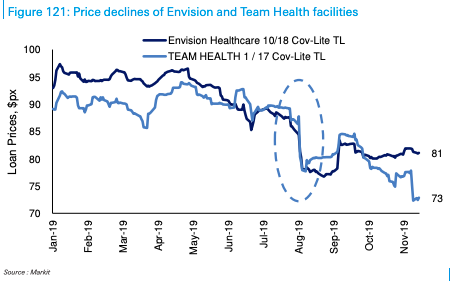
All this talk of reining in charges by out-of-network physicians has taken a financial toll on the massive debt piled on the physician staffing agencies by their private equity owners. The debt has fallen in value as proposals to protect patients from surprise bills raised concerns about whether the debt can be repaid. KKR’s 2018 leveraged buyout of Envision, for example, was financed in part by $5.4 billion in debt due in 2025. The financial times writes,11 the value of the debt “slid from almost 97 cents on the dollar at the start of May to just 87.8 cents on the dollar” in late July as talk of reining in charges for Envision’s services heated up. The slide continued even after the arbitration provision was added to the House No Surprises Act. By the end of August, Envision’s debt was trading at 77.3 cents on the dollar. TeamHealth saw the price of its $2.7 billion loan due in 2024 decline to 73 cents on the dollar, well below the 80 cents on the dollar threshold for distressed debt (see figure below).
Agreement on a joint House and Senate bipartisan bill by Senators Alexander and Murray and Congressmen Pallone and Walden nearly made it into the omnibus continuing resolution that passed in December 2019. It was stymied when Massachusetts Congressman Richard Neal, Chair of the House Ways and Means Committee, offered a last-minute alternative. The Neal bill protects consumers from surprise medical bills but requires disputes between providers and insurance companies to be resolved through arbitration. This, of course, is what the PE-owned staffing firms and the doctors’ practices they own lobbied for. Lack of support from the Democratic leadership in the Senate and the House delayed passage of the legislation. In his September 2019 fundraising report, Neal reported receipt of $29,000 from Blackstone, owner of TeamHealth.12 The value of Envision’s and TeamHealth’s debt recovered somewhat on this news but remains in the low 80s for Envision and in the 70s for TeamHealth.
Figure 1
Source: Deutsche Bank CLO Research and Markit
In the current legislative session, Congress is again working to pass legislation to protect patients from surprise medical bills. But the disagreements in Congress remain unresolved. On February 7, two House committees — Energy and Commerce, chaired by Pallone, and Ways and Means, chaired by Neal — released their proposals. The Senate Education and Labor Committee, chaired by Alexander, also released its proposal that day. The Ways and Means Committee’s proposal calls for arbitration when insurers and out-of-network providers fail to agree on payment. The other two proposals blend a benchmark rate and arbitration, allowing arbitration in some limited circumstances and requiring the arbitrator to start from a benchmark rate. Chances of a compromise bill emerging in this session of Congress do not look good as of this writing (mid-February 2020), and relief for insured patients from unexpected medical bills does not appear to be on the horizon. Real relief from surprise medical bills may reemerge in 2021. Credit markets appear to be pricing in that possibility.
American Time Use Survey. 2018. “AMERICAN TIME USE SURVEY EXTRACT BUILDER.” Minneapolis, MN: IPUMS. https://www.atusdata.org/atus/.
Baker, Dean and Cherrie Bucknor. 2015. “The Affordable Care Act: Still Family-Friendly.” Washington, DC: Center for Economic and Policy Research. https://cepr.net/blogs/cepr-blog/the-affordable-care-act-still-family-friendly.
Bureau of Labor Statistics. 2018a. “Data Retrieval: Labor Force Statistics (CPS).” Washington, DC: Bureau of Labor Statistics. https://www.bls.gov/webapps/legacy/cpsatab8.htm. Retrieved 2018-08-20.
——. 2018b. “Table 3. Total separations levels and rates by industry and region, seasonally adjusted.” Washington, DC: Bureau of Labor Statistics. https://www.bls.gov/news.release/jolts.t03.htm. Retrieved 2018-08-20.
Cebi, Merve. 2011. “Employer-Provided Insurance and Labor Supply of Married Women.” Working Paper No. 11-171, Kalamazoo, MI: W. E. Upjohn Institute for Employment Research.
Colman, Gregory and Dhaval Dave. “It’s about Time: Effects of the Affordable Care Act Dependent Coverage Mandate on Time Use.” Contemporary Economic Policy, No. 1, 2018, p. 44.
Current Population Survey. 2018. “CURRENT POPULATION SURVEY DATA FOR SOCIAL, ECONOMIC AND HEALTH RESEARCH.” Minneapolis, MN: IPUMS. https://cps.ipums.org/cps/.
Garthwaite, Craig, Tal Gross, and Matthew J. Notowidigdo. 2013. “Public Health Insurance, Labor Supply, and Employment Lock.” NBER Working Paper No. 19220, Cambridge, MA: NBER.
Gruber, Jonathan and Brigette C. Madrian. 2002. “Health Insurance, Labor Supply, and Job Mobility: A Critical Review of the Literature.” NBER Working Paper No. 8817, Cambridge, MA: NBER.